Exploring the Impact of Mosquito-Borne Diseases In 2025
Mosquito populations and mosquito-bite disease risks are always changing due to weather, urban development, targeted management efforts, and other factors. Year-to-year variation is normal, and the 2025 data from the Centers for Disease Control and Prevention (CDC) reflect several notable changes in reported cases compared to 2024:
- La Crosse Encephalitis: 203% increase; 194% increase in neuroinvasive
- St. Louis Encephalitis: 200% increase; 200% increase in neuroinvasive
- West Nile virus: 42% increase; 35% increase in neuroinvasive
Our 2025 year in review provides trends and insights that can help inform your mosquito management decisions in 2026.
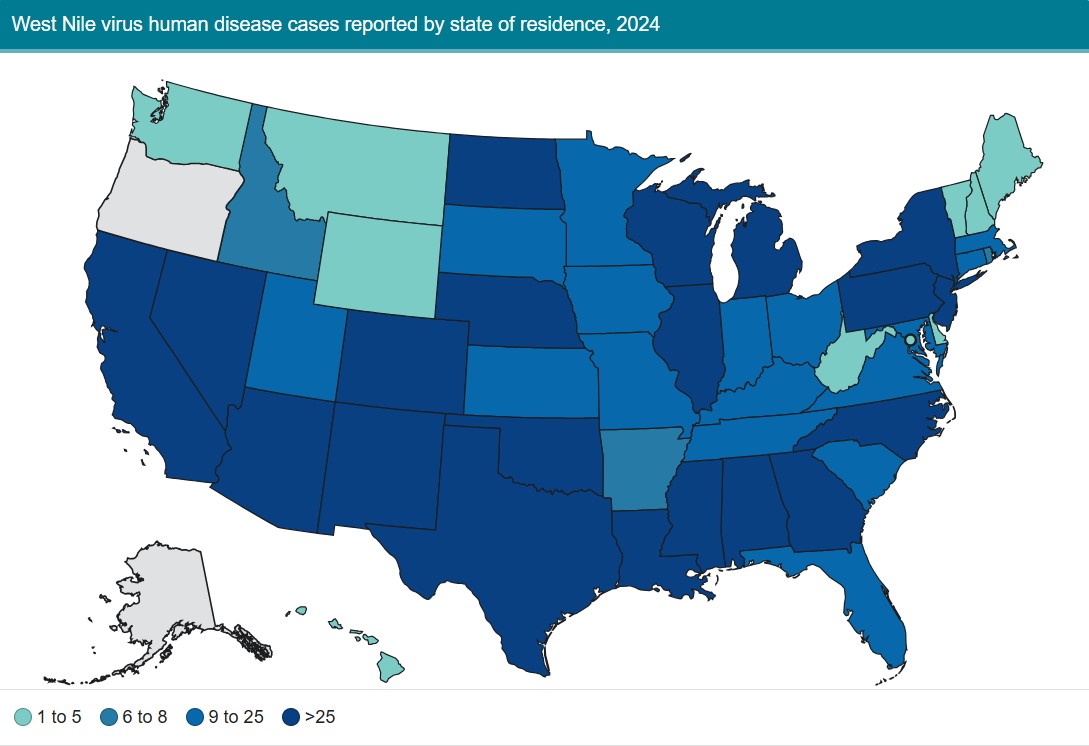
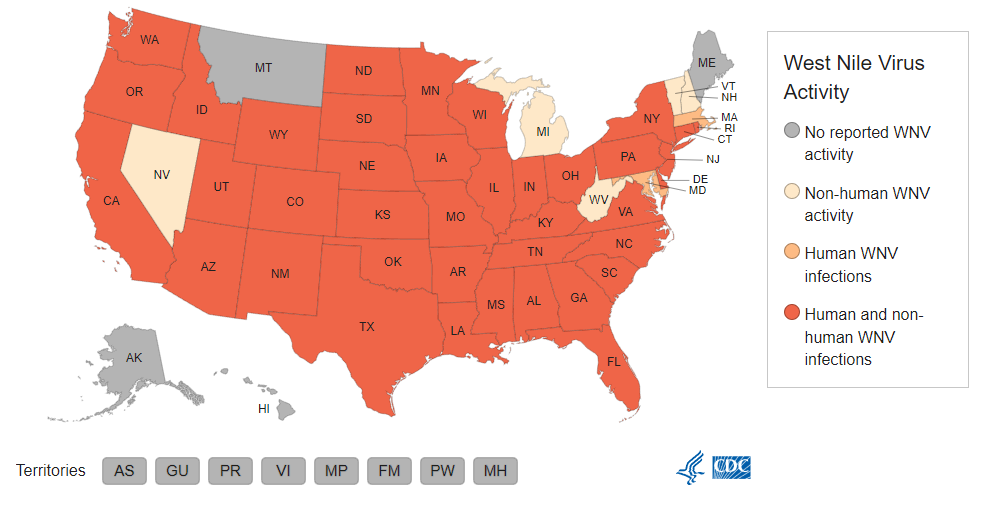
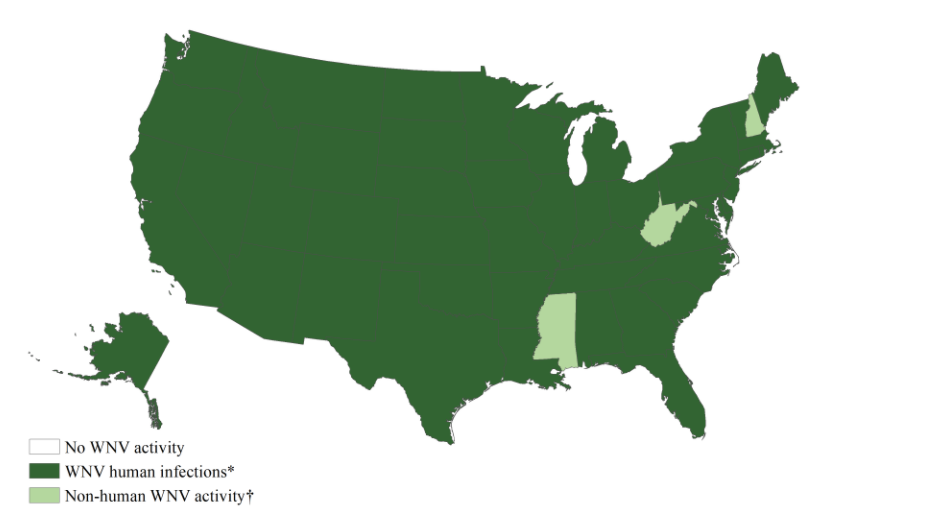
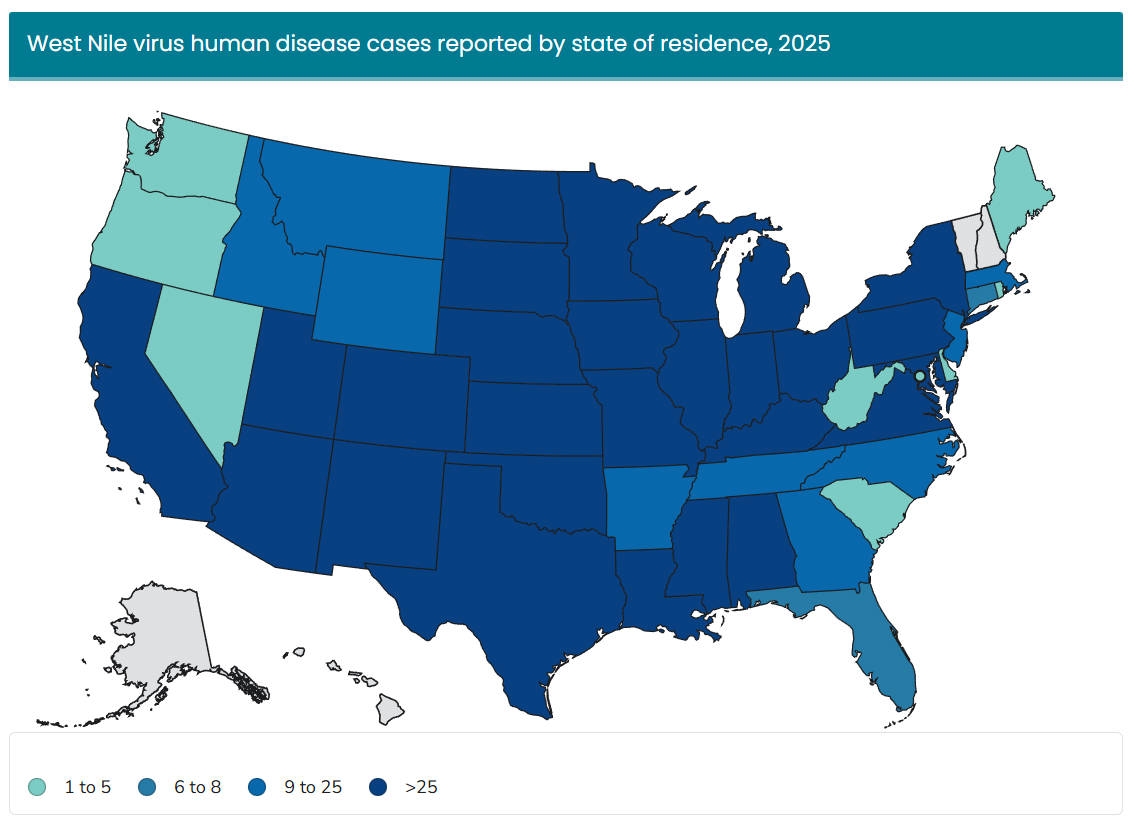
West Nile Virus (WNv)
OVERVIEW:
- The virus appeared in the U.S. in 1999, with the first case in New York City, leading to 62 human cases and 25 horse cases that year.
- WNv is now the most common mosquito-borne disease in the country, with an estimated 2,000 cases reported each year.
TRANSMISSION:
- The West Nile virus spreads primarily through mosquitoes that feed on infected birds, not through casual human-to-human contact.
- In the U.S., Culex pipiens, Culex tarsalis, and Culex quinquefasciatus are the primary vectors.
RISKS:
- Most cases are asymptomatic, but symptoms can include flu-like illness, fever, rash, headache, and neck stiffness.
- Severe infections can cause encephalitis (brain swelling), affect the central nervous system, and may be fatal. Approximately 1 in 150 infections becomes neuroinvasive.
Year-Over-Year Change in West Nile Virus Cases
Top 5 States for West Nile Virus Human Case Count
- Colorado (285)
- Illinois (149)
- Texas (127)
- Minnesota (122)
- California (112)
- *Data are current as of January 13, 2026.
**Total human disease cases include neuroinvasive and non-neuroinvasive disease cases.
Source: https://www.cdc.gov/west-nile-virus/data-maps/current-year-data.html
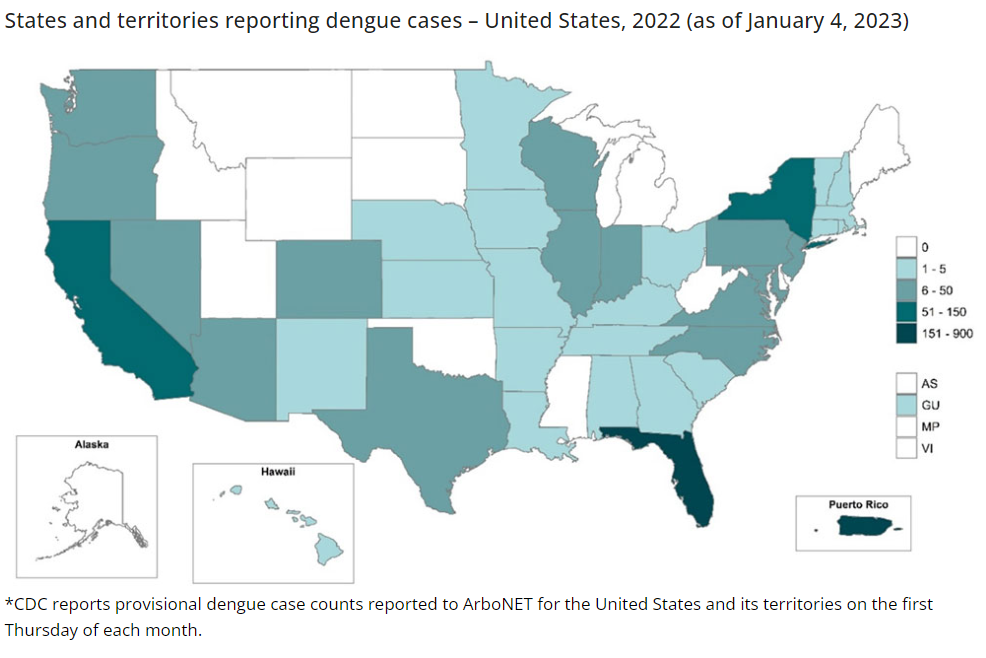
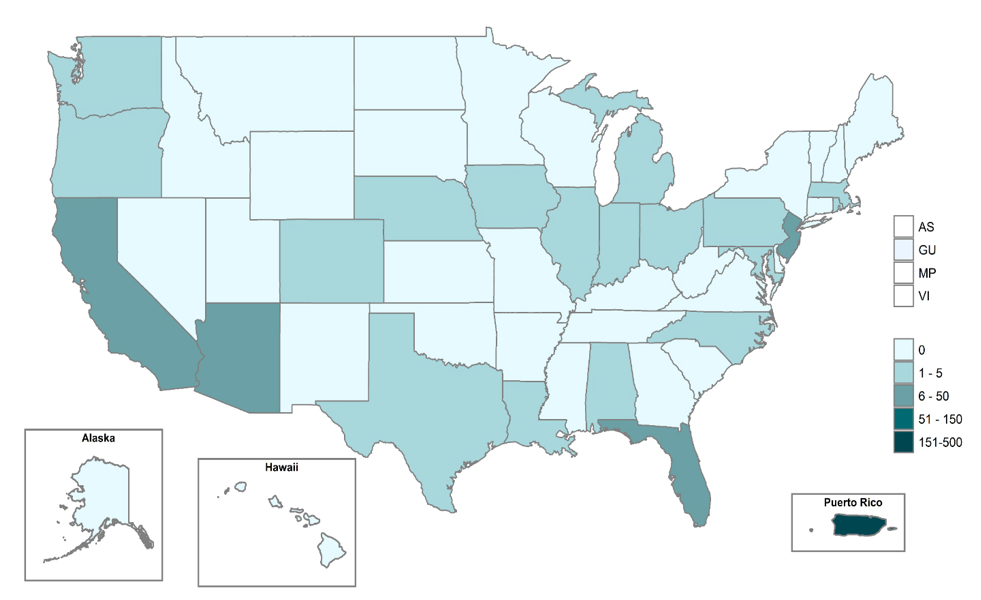
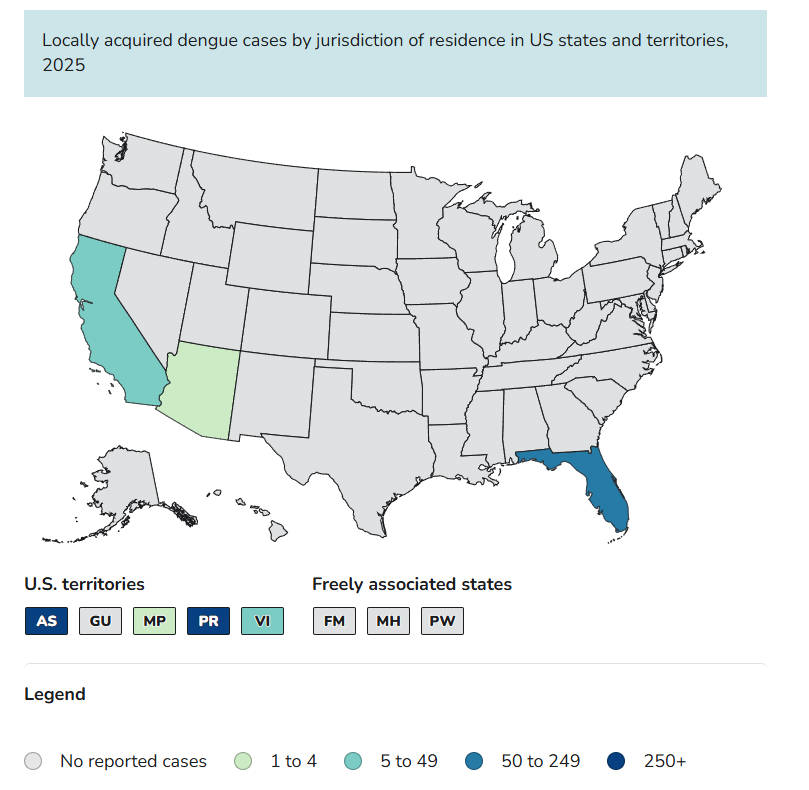
Dengue
NOTE: Most dengue cases in the 49 continental U.S. states are imported through travel. Although local transmission can occur, it is largely limited to U.S. territories and states where dengue is common. Below, cases are categorized separately as either locally acquired or travel-associated.
OVERVIEW
- Dengue is common in the U.S. territories of American Samoa, Puerto Rico, and the U.S. Virgin Islands.
- Most dengue cases reported in the 49 continental US states occur in travelers infected in areas with risk of dengue.
- Dengue has become the fastest-growing mosquito-transmitted disease, with nearly 400 million infections annually worldwide.
TRANSMISSION
- There are 4 common Dengue viruses, denoted as Dengue 1, 2, 3, and 4.
- Dengue is transmitted to humans through infected Aedes mosquitoes, specifically Aedes aegypti and Aedes albopictus.
RISKS
- Infection can cause “break-bone fever” (severe muscle/joint pain, high fever, rash, headache), with approximately 5% of cases developing severe dengue hemorrhagic fever, which can lead to internal bleeding and death.
- Severe cases are more likely in young children and older adults.
- The virus can be passed to fetuses during pregnancy.
The chart below provides a year-over-year comparison of locally acquired dengue cases to highlight changes in local transmission activity.
Year-Over-Year Change in Dengue Cases
Top 5 States for Dengue Human Case Count
- Puerto Rico (3,370)
- American Samoa (324)
- Florida (60)
- U.S. Virgin Islands (47)
- California (6)
- *Data are current as of January 13, 2026.
**All dengue cases by jurisdiction of residence in US states and territories
Source: https://www.cdc.gov/dengue/data-research/facts-stats/current-data.html
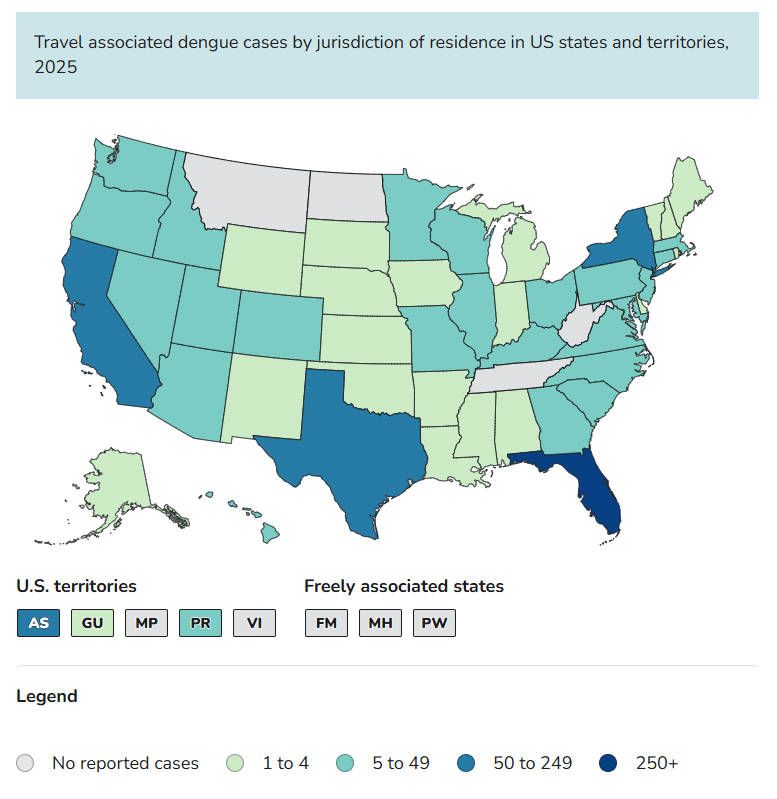
The chart below provides a year-over-year comparison of travel-associated dengue cases to highlight changes in travel-related exposure patterns.
Year-Over-Year Change in Dengue Cases
Top 5 States for Dengue Human Case Count
- Florida (417)
- California (164)
- New York (81)
- American Samoa (77)
- Texas (58)
- *Data are current as of January 13, 2026.
**All dengue cases by jurisdiction of residence in US states and territories
Source: https://www.cdc.gov/dengue/data-research/facts-stats/current-data.html
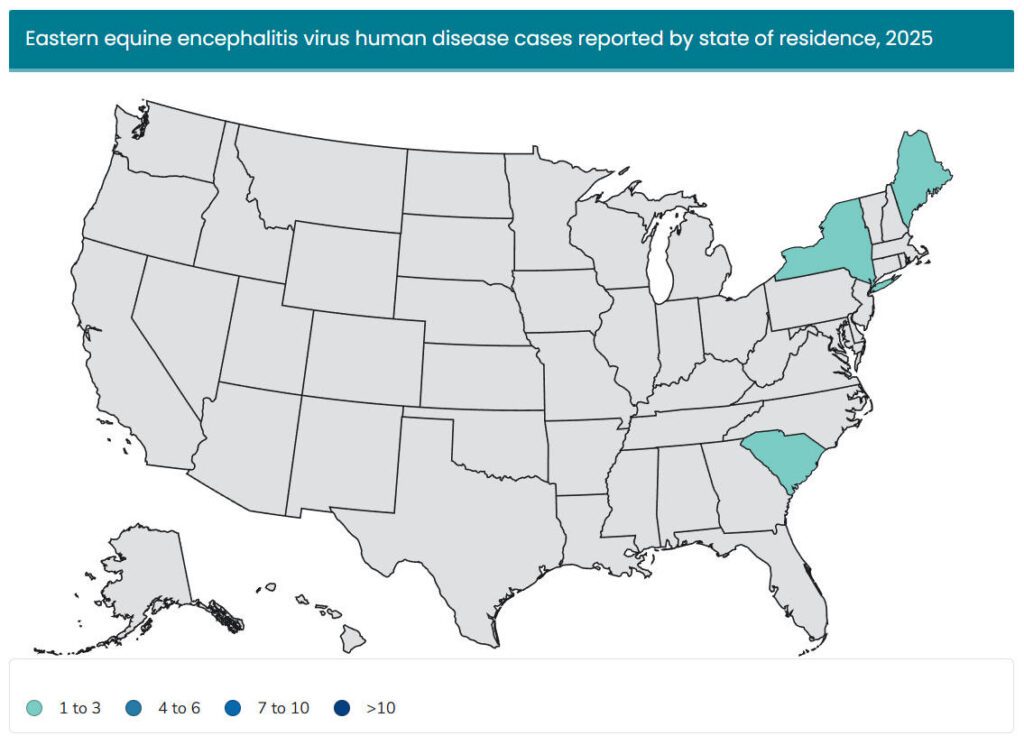
Eastern Equine Encephalitis (EEE)
OVERVIEW
- Eastern Equine Encephalitis (EEE) was first recognized in horses in 1831, with the first confirmed human cases in 1938.
- Today, EEE is found in North, Central, and South America, as well as the Caribbean.
TRANSMISSION
- Culiseta melanura primarily infects birds, while bridge vectors like Coquillettidia pertubans, Aedes sollicitans, and Ochlerotatus canadensis transmit it to humans and horses.
- People living or working near wetlands and swamps are at higher risk, and infections occur mainly during the summer months.
RISKS
- Severe cases involve brain and spinal cord inflammation, with sudden high fever, stiff neck, disorientation, seizures, and coma.
- Only about 5% of EEE infections lead to severe encephalitis; of those, 33% die, making it the deadliest arbovirus in the U.S.
- The elderly (50+) and children (15 and younger) are most at risk for developing encephalitis.
- There is no vaccine or antiviral treatment for humans.
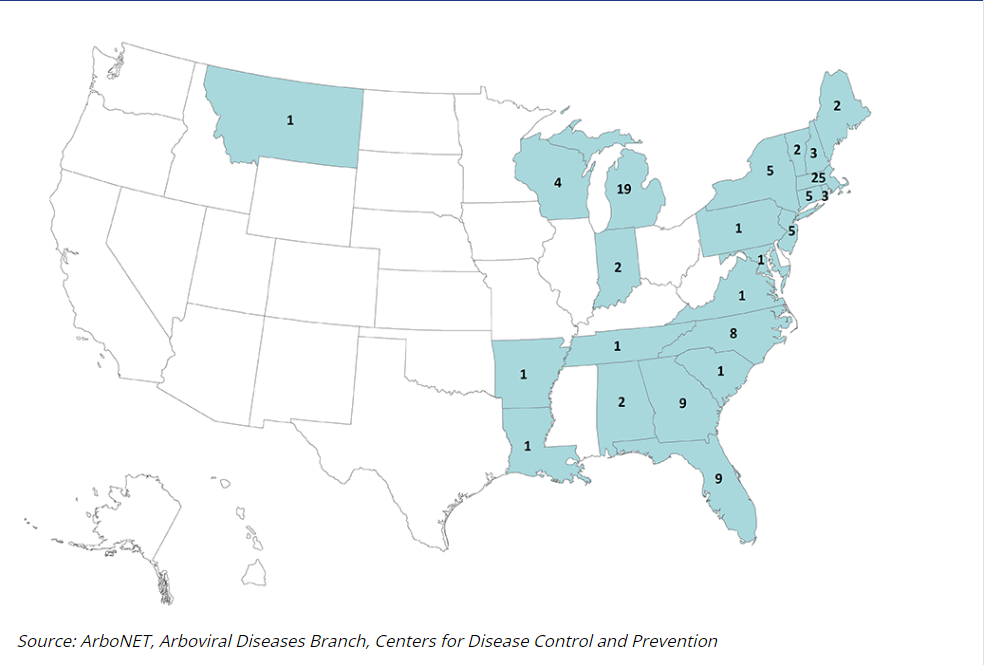
Year-Over-Year Change in Eastern Equine Encephalitis Cases
Top 3 States for Eastern Equine Encephalitis Human Case Count
- Main (1)
- New York (1)
- South Carolina (1)
- *Data are current as of January 13, 2026.
**Total human disease cases include neuroinvasive and non-neuroinvasive disease cases.
Source: https://www.cdc.gov/eastern-equine-encephalitis/data-maps/current-year-data.html
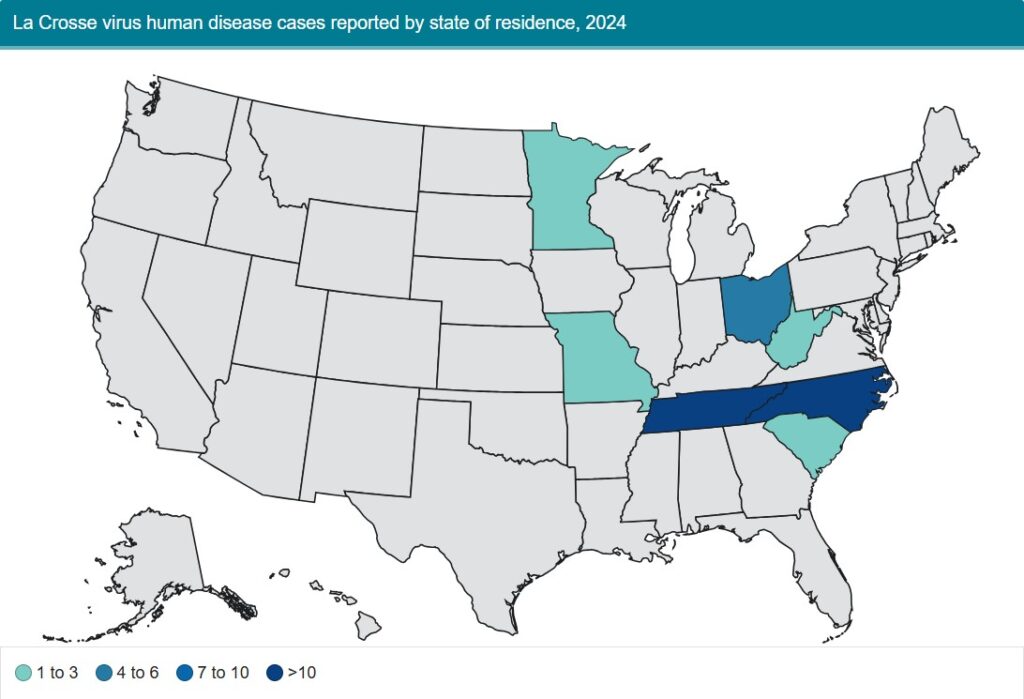
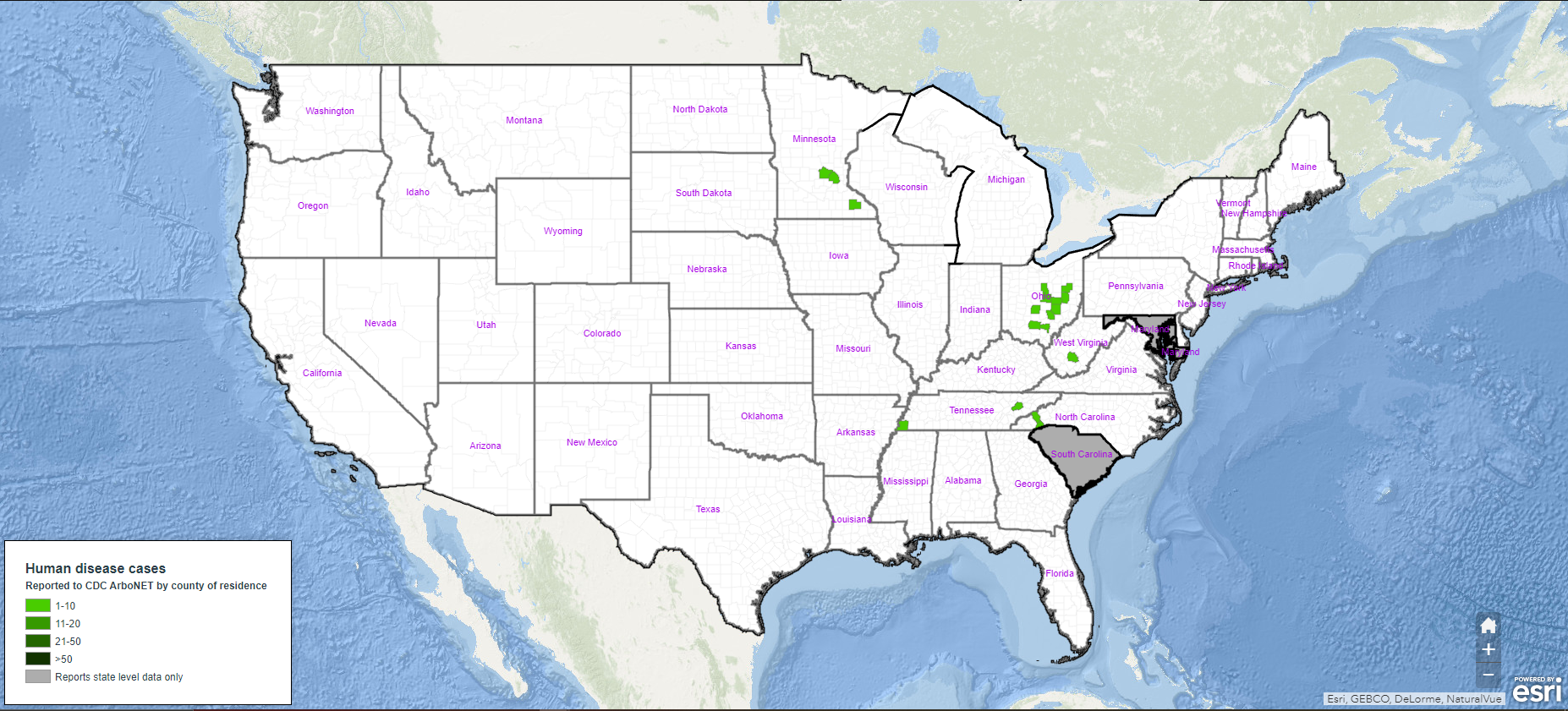
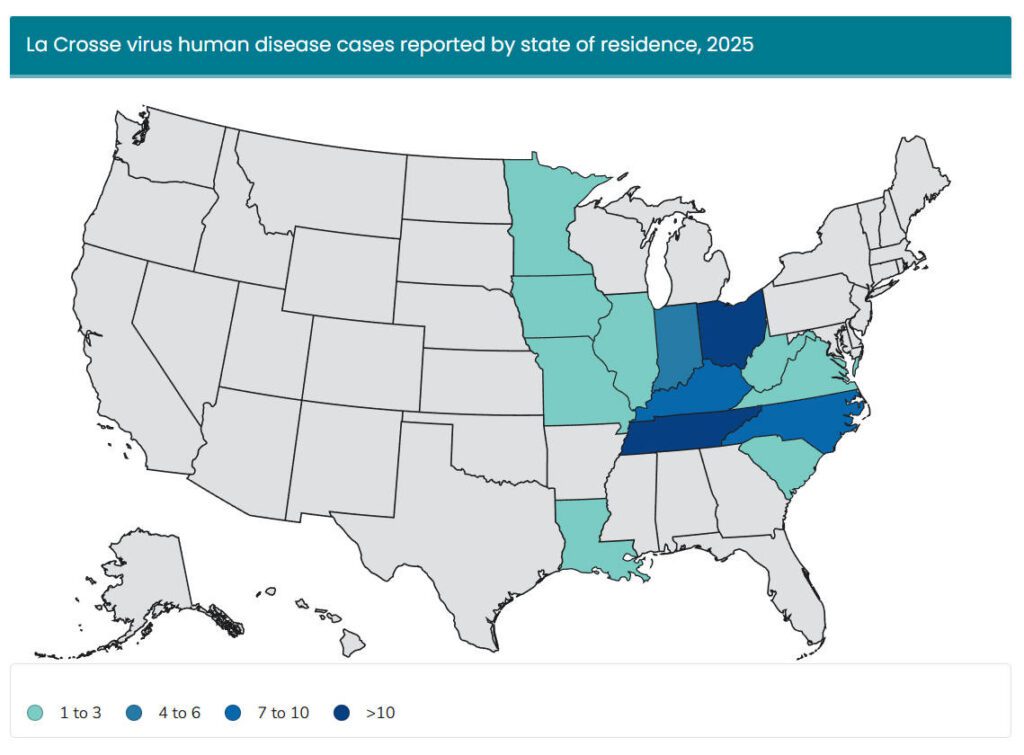
La Crosse Encephalitis (LAC)
OVERVIEW
- La Crosse Encephalitis (LAC) was first identified in the United States in 1964.
- Most commonly reported in the upper Midwest and Mid-Atlantic states, including Ohio, West Virginia, and Minnesota.
TRANSMISSION
- Primarily spread by the Eastern treehole mosquito, Aedes triseriatus.
- Aedes triseriatus can pass the virus to its offspring, which allows it to persist across mosquito generations.
- Reservoir hosts like chipmunks and squirrels are also carriers.
RISKS
- LAC primarily affects children under 16, making it a rare but serious pediatric mosquito-borne disease.
- Flu-like symptoms, including headache, fever, nausea, vomiting, and fatigue, may appear 5-15 days after infection.
- Severe infections can cause brain inflammation, seizures, cognitive impairment, vision loss, paralysis, or coma, though mortality is less than 1%.
- There is no vaccine or antiviral treatment.
Year-Over-Year Change in La Crosse Encephalitis Cases
Top States for La Crosse Encephalitis Human Case Count
- Ohio (53)
- Tennessee (26)
- Kentucky (7) / South Carolina (7)
- Indiana (4)
- West Virginia (2)
- *Data are current as of January 13, 2026.
**Total human disease cases include neuroinvasive and non-neuroinvasive disease cases.
Source: https://www.cdc.gov/la-crosse-encephalitis/data-maps/current-year-data.html
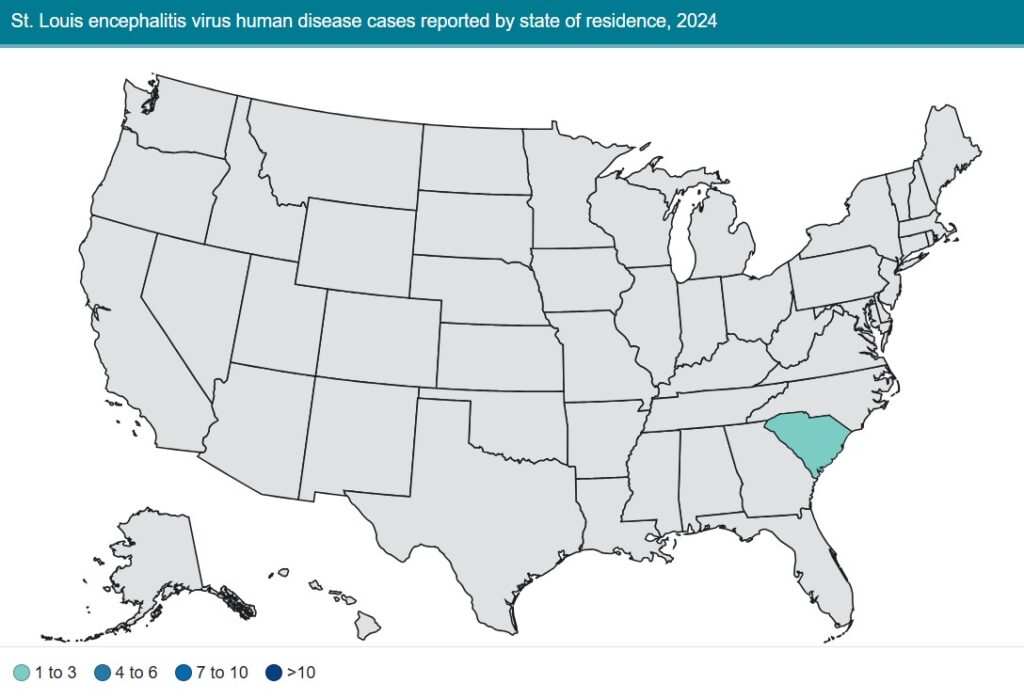
St. Louis Encephalitis (SLEV)
OVERVIEW
- The St. Louis encephalitis virus (SLEV) was first recognized in 1933 during a St. Louis, Missouri, epidemic that resulted in over 1,000 cases of encephalitis.
- Before West Nile virus appeared in 1999, SLEV was considered the most significant epidemic mosquito-borne virus in the U.S., with the last major epidemic in 1975 along the Ohio–Mississippi River Basin (nearly 2,000 cases, 142 deaths).
TRANSMISSION
- Primary vectors include Culex pipiens, Culex quinquefasciatus, Culex tarsalis, and Culex nigripalpus.
- Wild birds, such as blue jays, sparrows, robins, and pigeons, act as amplifying hosts, but typically remain asymptomatic.
RISKS
- Most infections are asymptomatic; severe cases can cause high fever, neck stiffness, disorientation, coma, or death, with mortality ranging from 3-30% depending on age.
- Adults over 50 are more likely to develop severe disease, with mortality between 7-24%, while those under 50 generally face less than 5% mortality.
Year-Over-Year Change in St. Louis Encephalitis Cases
Top State for St. Louis Encephalitis Human Case Count
- Arizona (3)
-
*Data are current as of January 13, 2026.
**Total human disease cases include neuroinvasive and non-neuroinvasive disease cases.
Source: https://www.cdc.gov/sle/data-maps/current-year-data.html

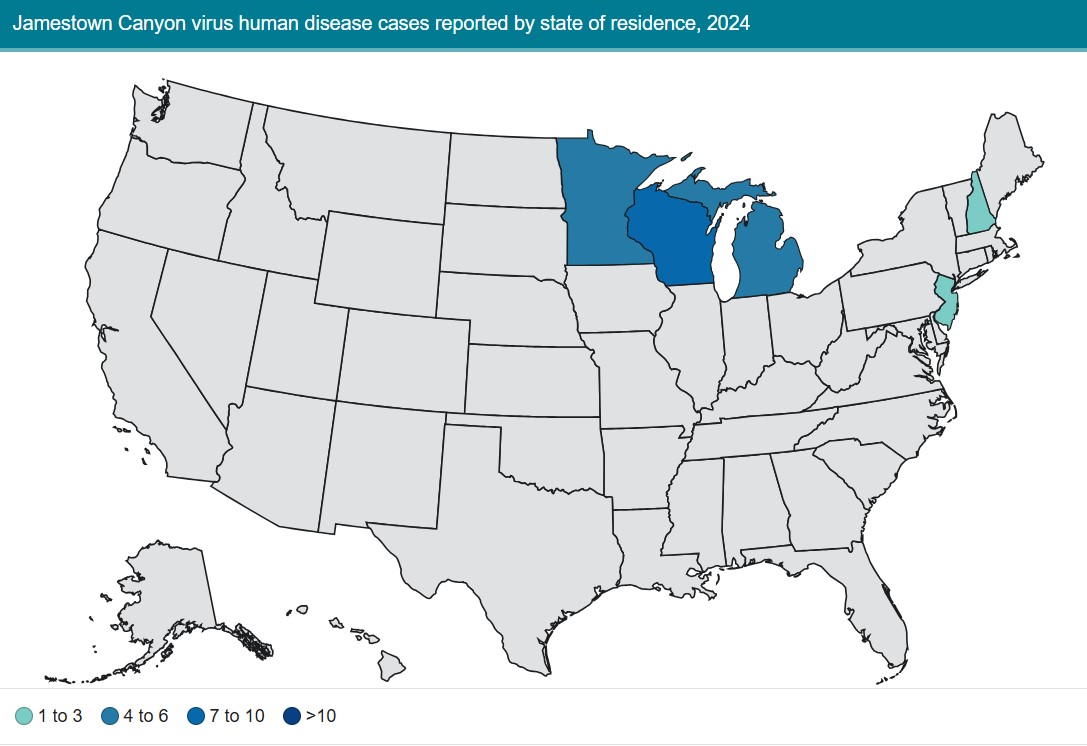
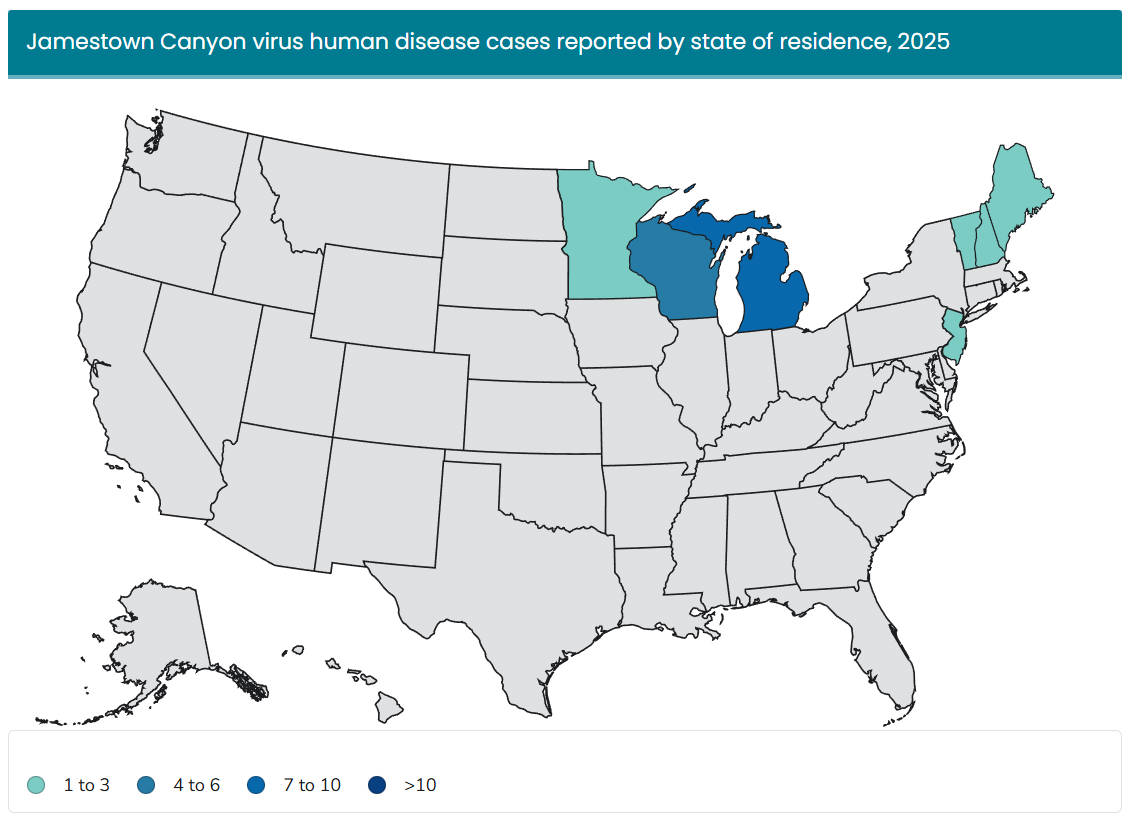
Jamestown Canyon virus (JCV)
OVERVIEW
- Jamestown Canyon virus (JCV) was first discovered in Culiseta mosquitoes in Jamestown, Colorado, in 1961.
- It is found throughout much of the U.S., with most cases reported in the upper Midwest.
TRANSMISSION
- Various mosquito species serve as vectors: Aedes, Culex, Coquillettidia.
- JCV can be transmitted from mosquito parents to offspring.
- Deer often serve as the amplifying host, while humans are “dead-end” hosts and cannot transmit the virus to other mosquitoes.
RISKS
- Symptoms include fever, headache, and fatigue.
- Most JCV cases are neuroinvasive. About 68% of reported infections affect the nervous system, with symptoms ranging from fever and rash to meningitis or encephalitis.
- No treatment currently exists.
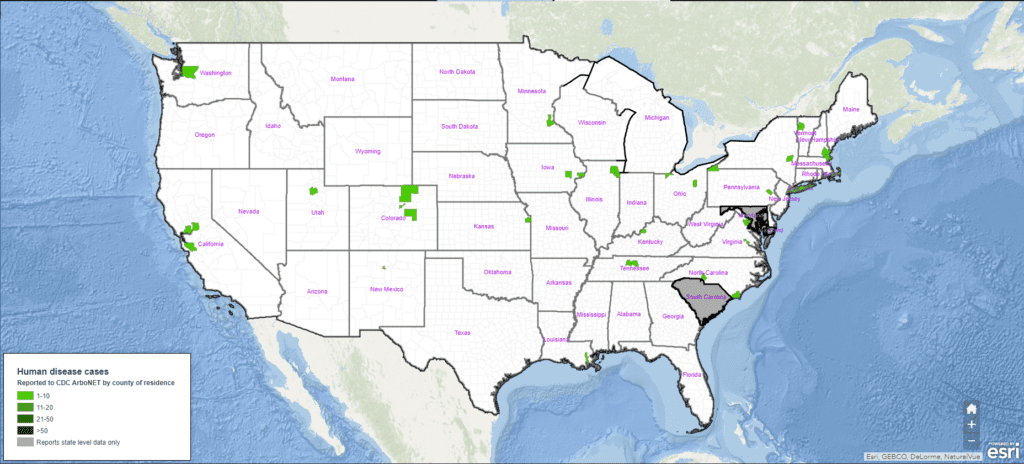
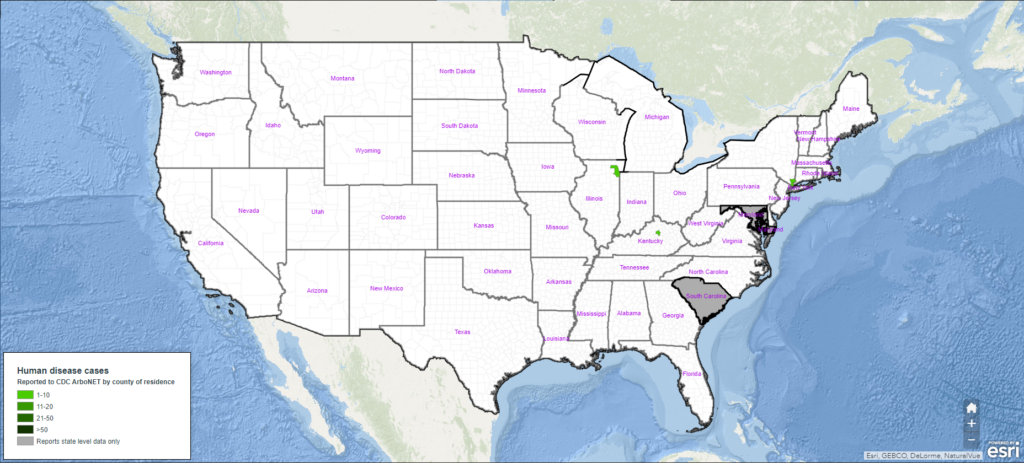
Year-Over-Year Change in Jamestown Canyon Virus Cases
Top States for Jamestown Canyon Virus Human Case Count:
- Michigan (10)
- Wisconsin (5)
- Minnesota (2) / New Jersey (2)
- *Data are current as of January 13, 2026.
**Total human disease cases include neuroinvasive and non-neuroinvasive disease cases.
Source: https://www.cdc.gov/jamestown-canyon/data-maps/current-year-data.html
DATA IS THE BACKBONE OF EFFECTIVE MOSQUITO CONTROL PROGRAMS
Data from 2025 and prior years reveal that disease risks are continually shifting and evolving across the country. Protecting our local communities not only requires reactive solutions but also tailored, preventative strategies driven by data.
Integrated Mosquito Management programs incorporate data and insights from surveillance, disease testing, and mosquito control at every lifecycle stage—all supported by robust public education initiatives—to stay ahead of mosquito-borne disease threats.
Whether you need full program management or expert support, VDCI has the technical expertise to partner with local leaders and jurisdictions. Contact our mosquito management experts today to help curb the spread of mosquito-borne diseases in 2026.
SOURCES
1. U.S. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/
VDCI Wants To Make Your Community Safer. How Can We Help?
Speak to an expert about implementing an IMM program.
Fill out the information below, and one of our experts will follow up with you shortly.
 Since 1992, Vector Disease Control International (VDCI) has taken pride in providing municipalities, mosquito abatement districts, industrial sites, planned communities, homeowners associations, and golf courses with the tools they need to run effective mosquito control programs. We are determined to protect the public health of the communities in which we operate. Our mosquito control professionals have over 100 years of combined experience in the field of public health, specifically vector disease control. We strive to provide the most effective and scientifically sound mosquito surveillance and control programs possible based on an Integrated Mosquito Management approach recommended by the American Mosquito Control Association (AMCA) and Centers for Disease Control and Prevention (CDC). VDCI is the only company in the country that can manage all aspects of an integrated mosquito management program, from surveillance to disease testing to aerial application in emergency situations.
Since 1992, Vector Disease Control International (VDCI) has taken pride in providing municipalities, mosquito abatement districts, industrial sites, planned communities, homeowners associations, and golf courses with the tools they need to run effective mosquito control programs. We are determined to protect the public health of the communities in which we operate. Our mosquito control professionals have over 100 years of combined experience in the field of public health, specifically vector disease control. We strive to provide the most effective and scientifically sound mosquito surveillance and control programs possible based on an Integrated Mosquito Management approach recommended by the American Mosquito Control Association (AMCA) and Centers for Disease Control and Prevention (CDC). VDCI is the only company in the country that can manage all aspects of an integrated mosquito management program, from surveillance to disease testing to aerial application in emergency situations.