How Data Collection and Testing Help Reduce Mosquito-Borne Diseases
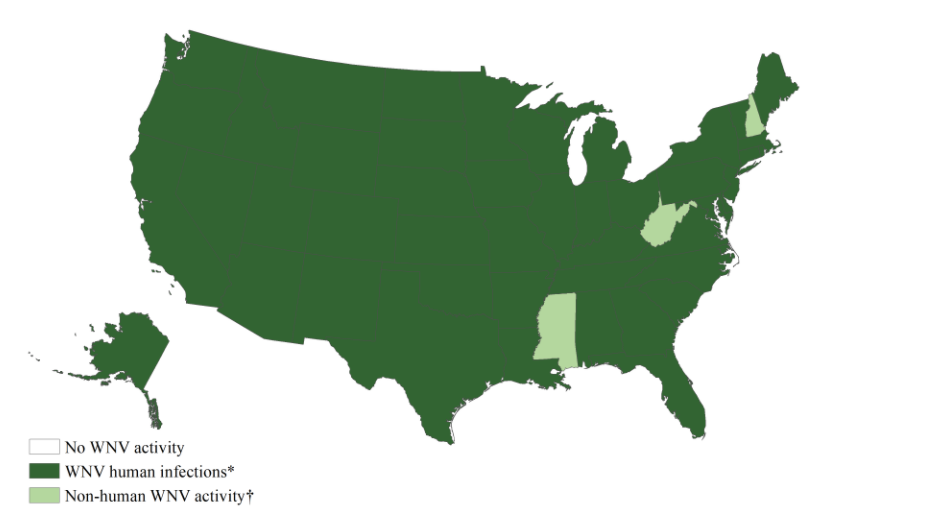
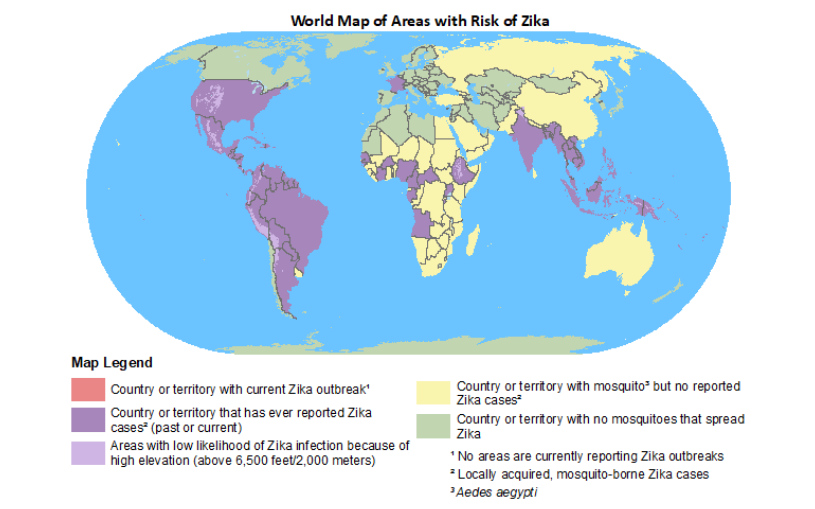
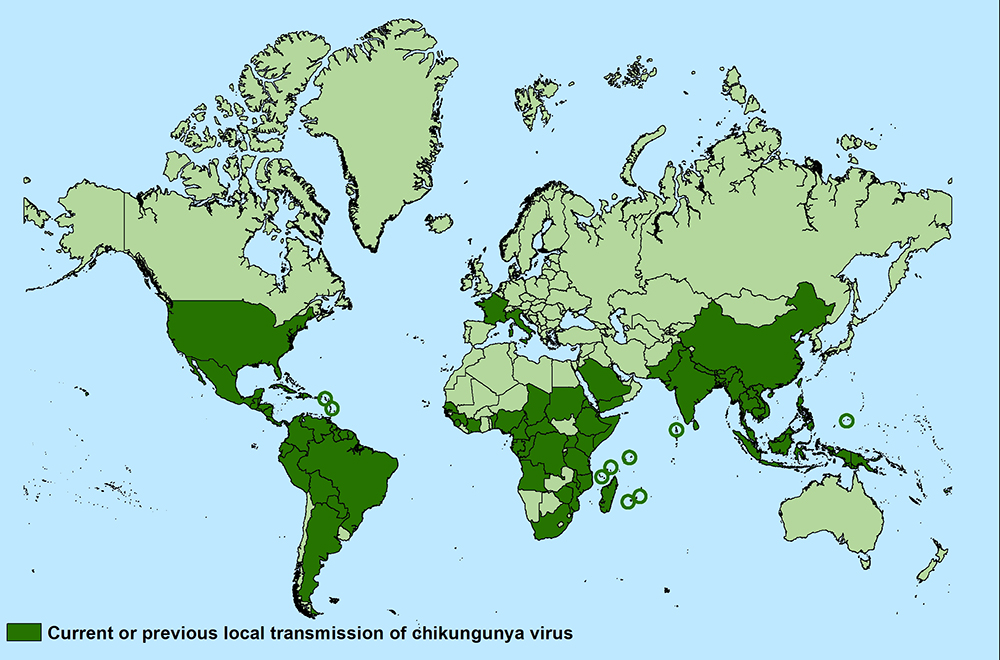
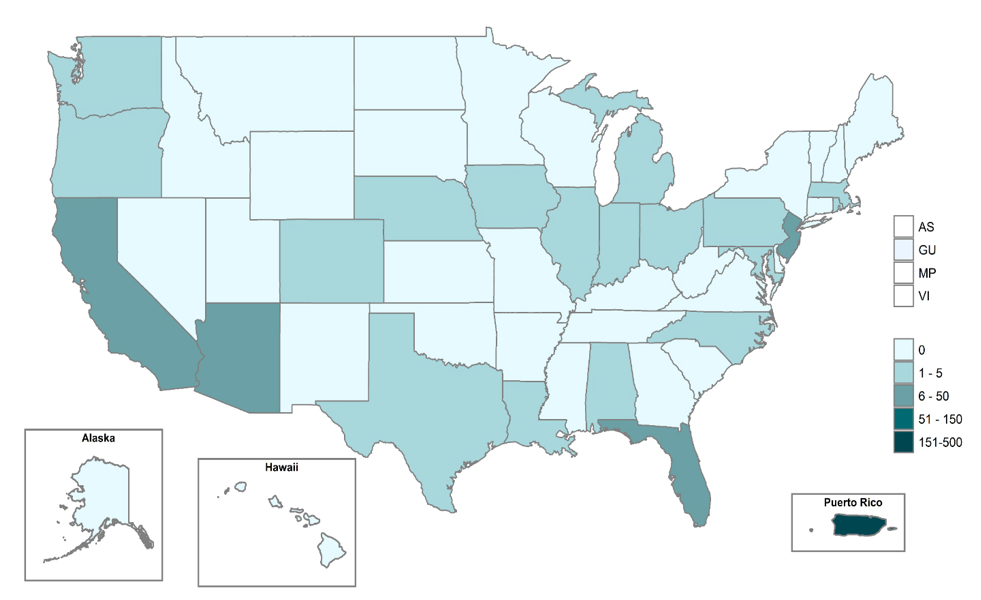
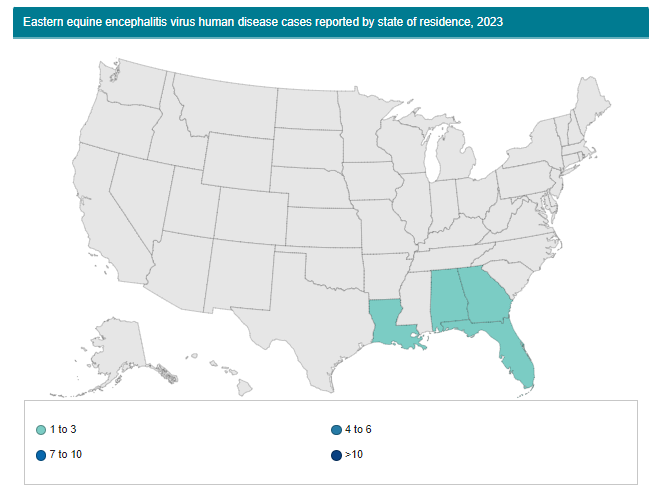
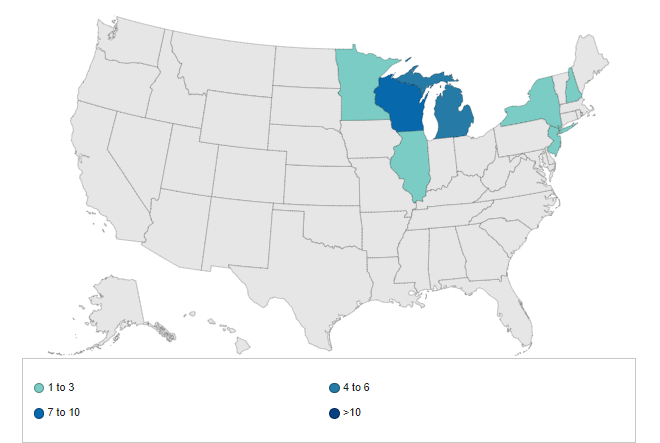
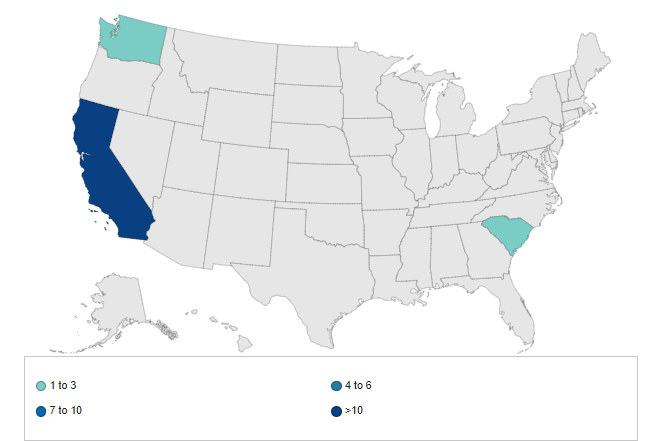
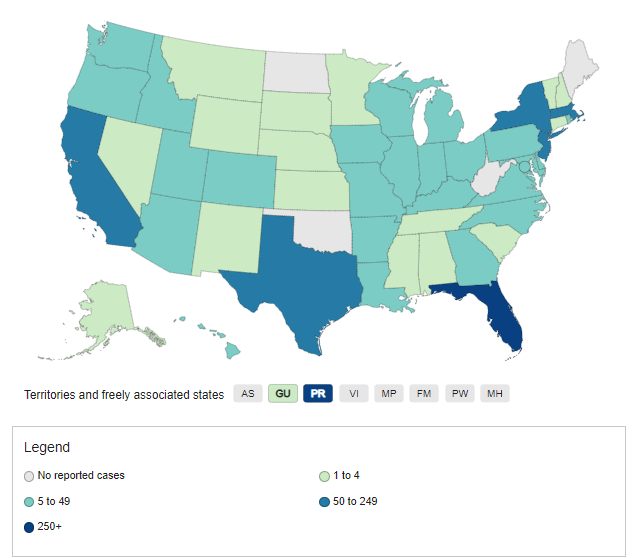
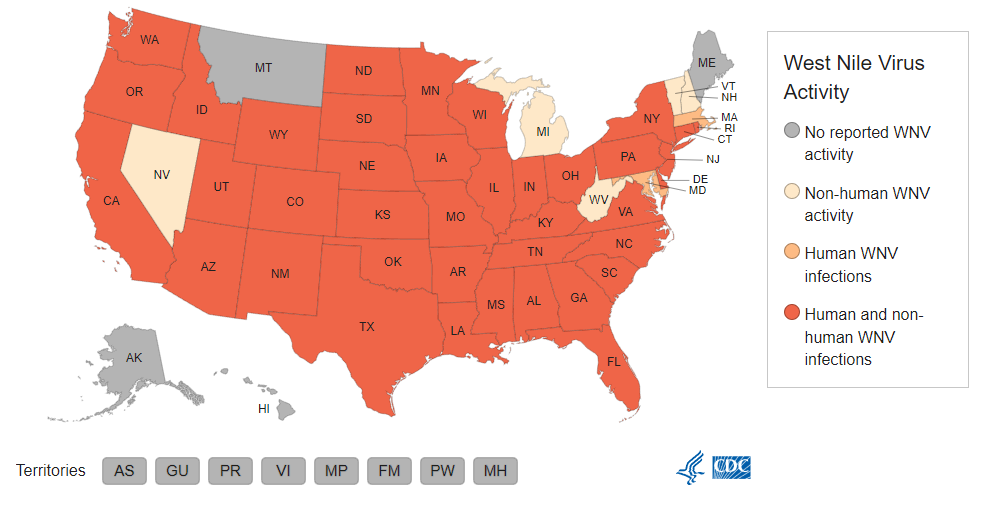
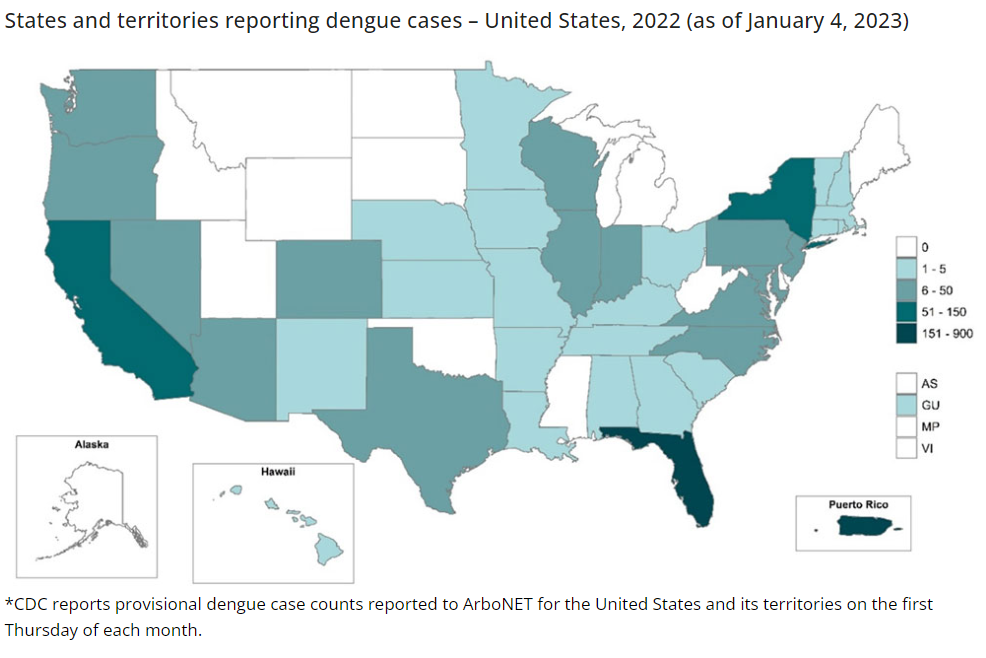
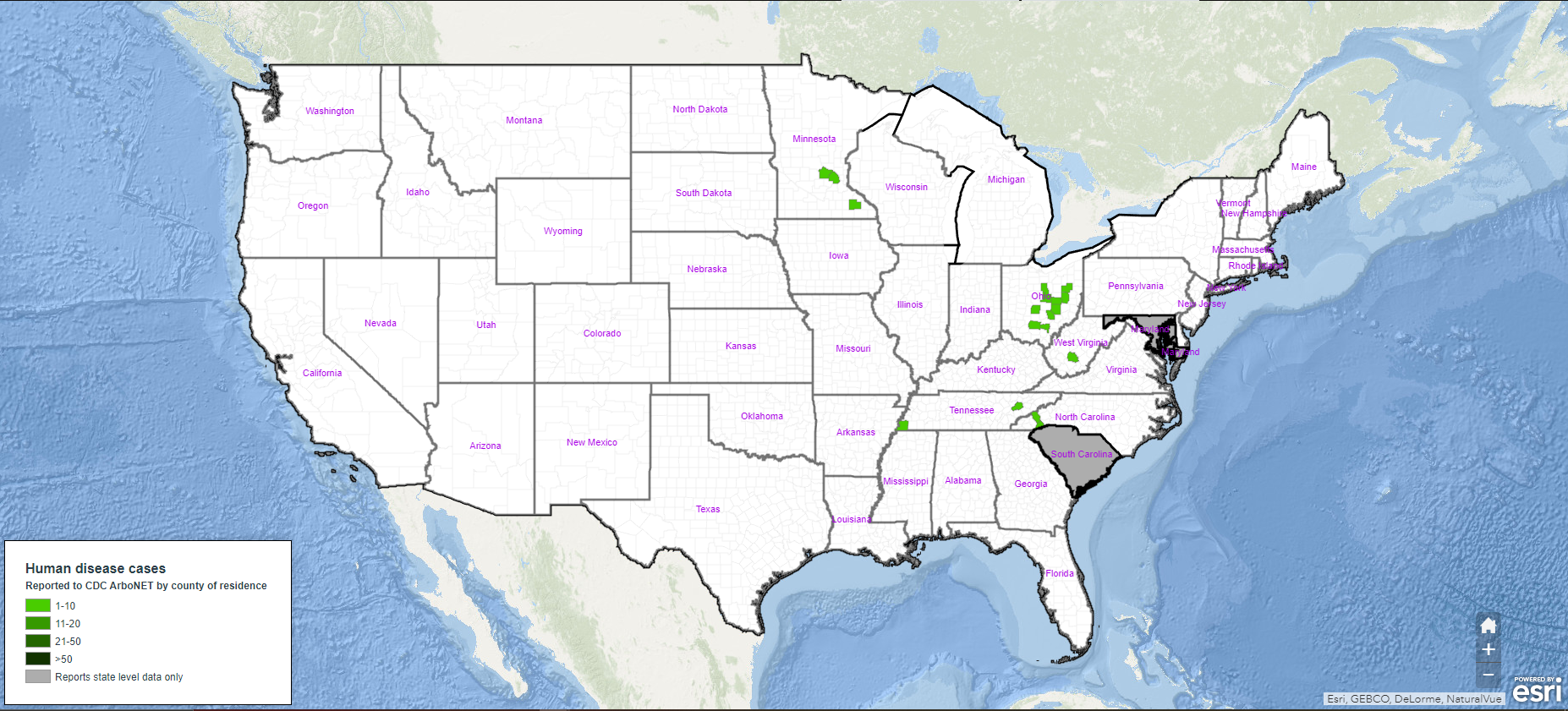
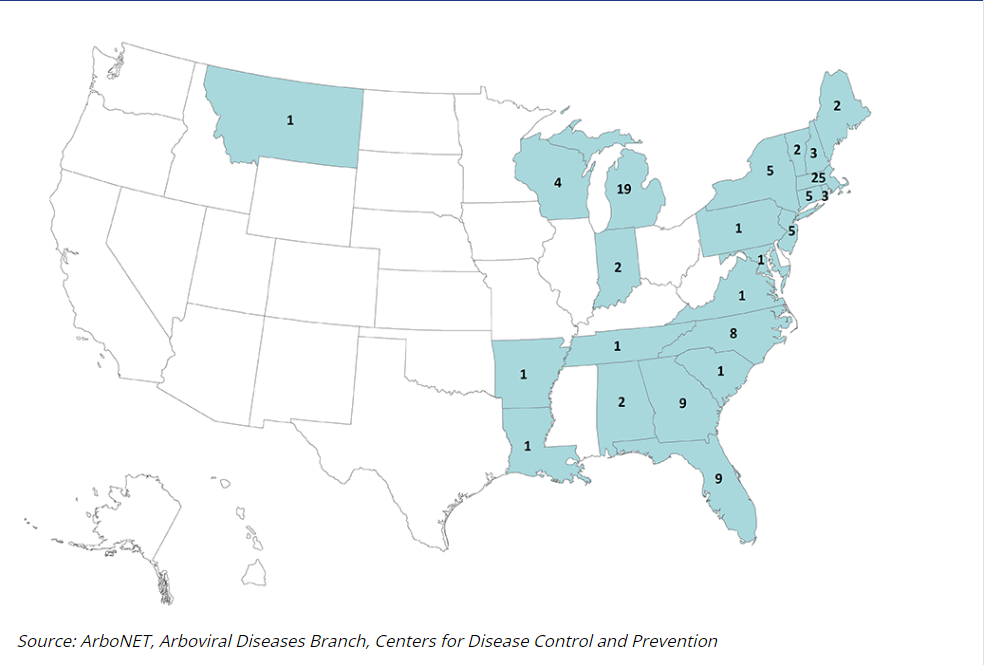
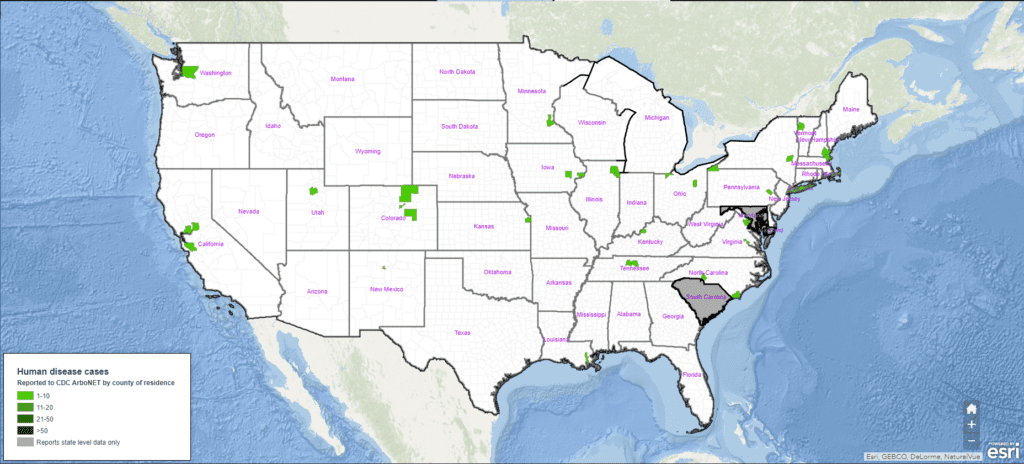
Mosquitoes are known to transmit several dangerous diseases that can pose a threat to human health. In the United States, mosquito-borne diseases such as West Nile virus, Eastern equine encephalitis virus, and dengue have all caused significant harm to communities nationwide – making the prevention of mosquito-borne diseases crucial for helping keep citizens safe.
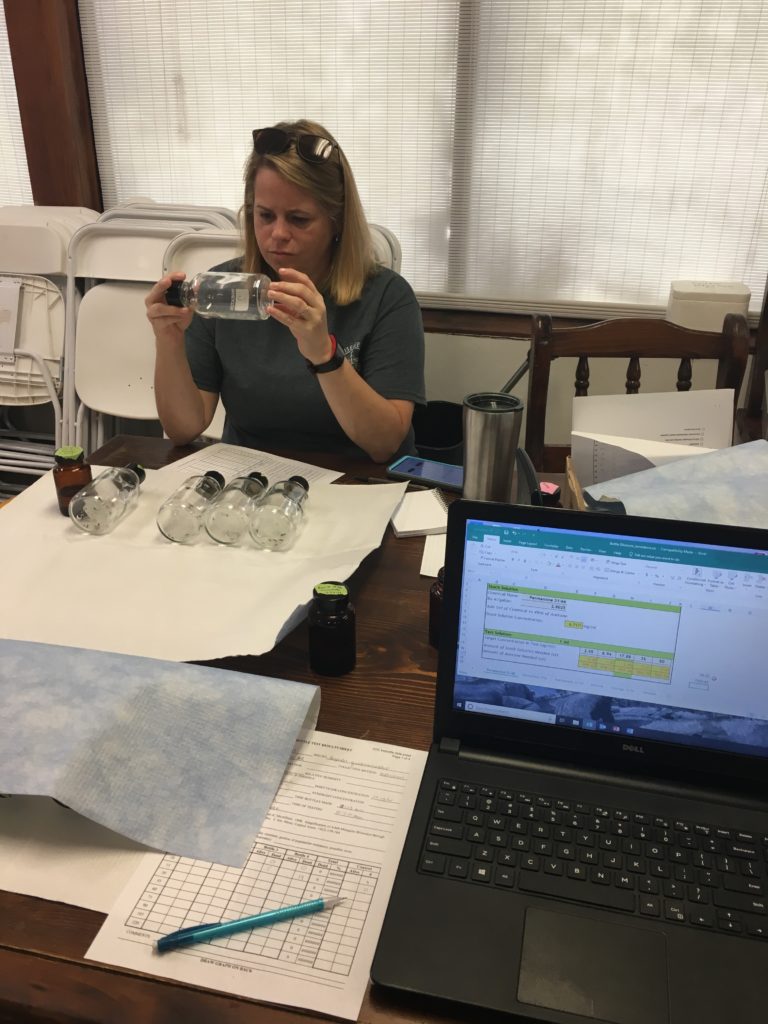
Proactively reducing the spread of these diseases starts with effective mosquito surveillance as part of an Integrated Mosquito Management (IMM) plan. Once adult mosquitoes are collected from various traps, they are sorted, identified, and analyzed in a lab where they undergo several tests, including disease testing. By testing adult mosquitoes for diseases, we can identify areas where disease-carrying mosquitoes are present and take appropriate action to reduce their population – ultimately reducing the spread of mosquito-borne diseases.

How Mosquito-Borne Disease Testing Works
Integrated Mosquito Management plans require extensive knowledge of mosquito species, breeding activities, and population dynamics to be successful. By conducting regular adult mosquito surveillance, experts can steadily monitor local populations, allowing us to detect mosquito-borne diseases weeks before they can be transmitted to humans or animals. Here’s how the disease testing process works:
- Our expert entomologists strategically set adult mosquito traps throughout a given area. Various mosquito traps are used depending on what information is desired. Each trap has its own unique advantages, many attract specific mosquito species, thereby focusing efforts to collect certain mosquito species that are more likely to carry disease. Traps are typically set weekly for regular population monitoring.
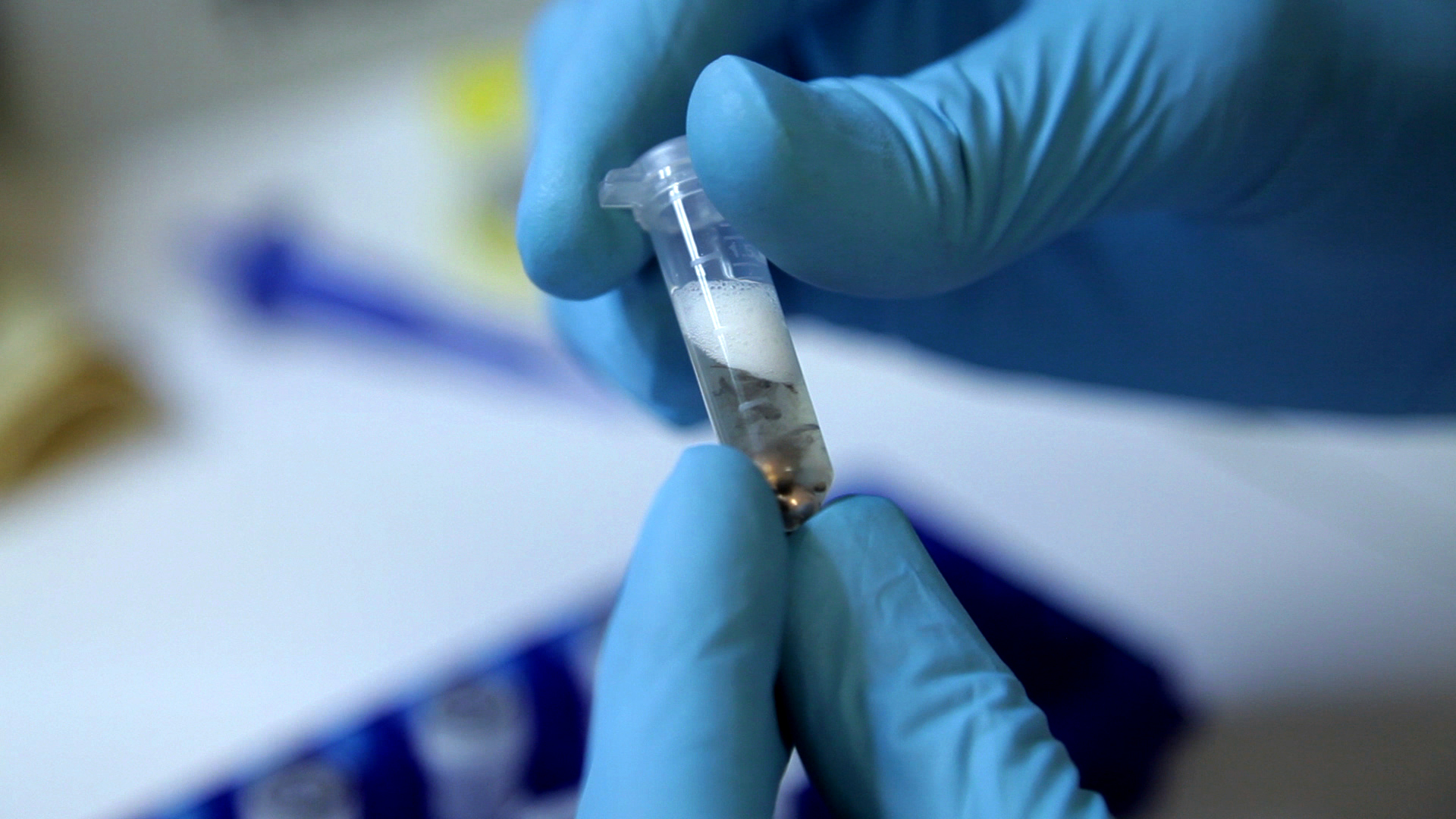
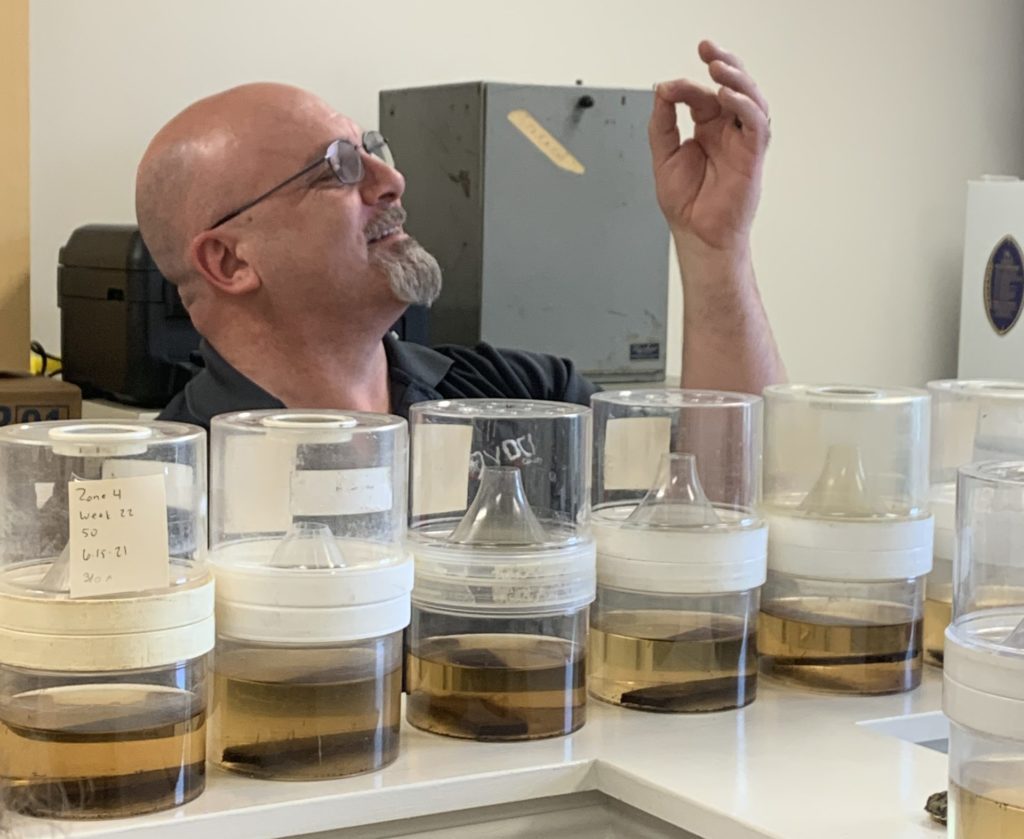
- Once a mosquito sample is collected, our entomologists will take them back to the lab for mosquito-borne disease testing.
- To identify which diseases are present in mosquito populations, our laboratory technicians will run PCR and RAMP® WNv tests. PCR tests allow us to detect different pathogens that are present inside the mosquito, while RAMP® tests are designed to detect West Nile virus, a commonly found mosquito-borne disease in the U.S.
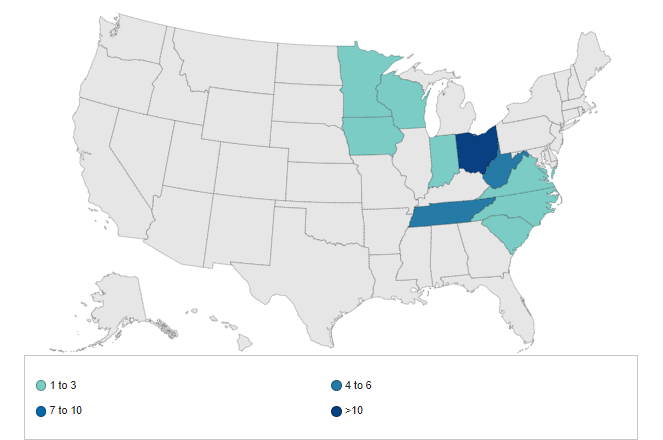
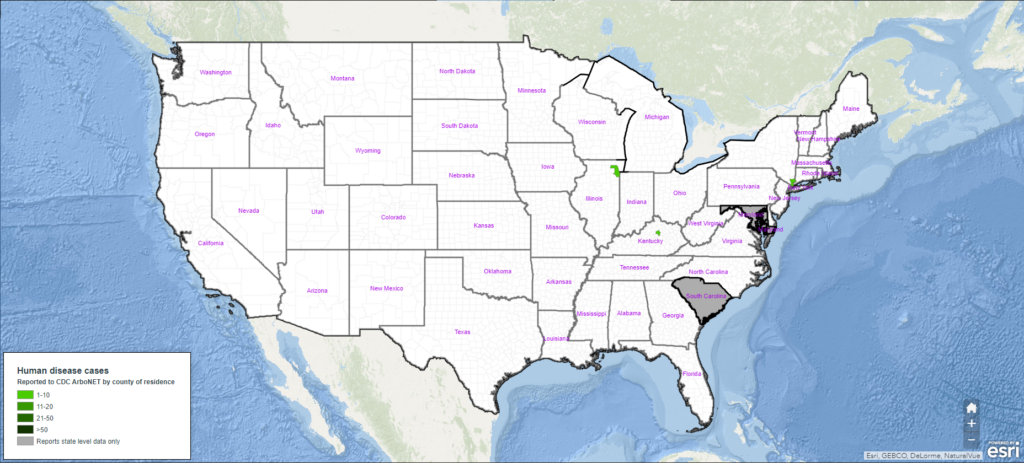
- If a mosquito sample tests positive for any mosquito-borne diseases, our entomologists will report the results to all appropriate local and state health departments. With this data, experts can determine the severity of a disease outbreak and respond with effective mosquito management solutions. This often involves returning to the area where the sample was collected and employing adult and larval mosquito control efforts.

Testing Best Practices
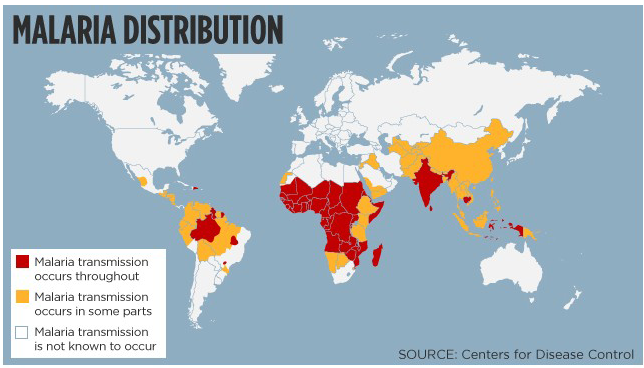
Mosquito-borne disease testing is crucial for helping support effective and environmentally responsible mosquito control. It’s important to follow industry best practices when testing mosquitoes for diseases such as West Nile and malaria.
- Test mosquitoes regularly to ensure we detect the presence of mosquito-borne diseases in a timely manner.
- Test mosquitoes trapped in various parts of the community to ensure we are casting a wide net for mosquito surveillance in the whole community.
- Use mosquito-borne disease testing results to drive IMM programs and reduce the spread of disease.
When a mosquito pool tests positive for a disease, the results of these tests are immediately communicated to government and health officials. This allows decision-makers to act quickly to reduce the spread of mosquito-borne diseases within their communities. By following these best practices, we can arm public officials with the knowledge they need to make control decisions to reduce the spread of mosquito-borne diseases.

Why Mosquito-Borne Disease Testing and Surveillance Matters
Mosquito-borne diseases can have severe consequences on the health and well-being of our communities nationwide. These diseases are transmitted through mosquito bites and can cause symptoms ranging from fever, rash, and neurological problems. Mosquito-borne disease testing and mosquito surveillance provide data and insights to drive a more effective IMM plan that works to reduce mosquito breeding sites and control both nuisance and disease-carrying mosquitoes.
A successful IMM program involves more than mosquito-borne disease testing. Several key pillars, including adult mosquito and larval surveillance, employing a variety of control strategies, and implementing public education within the community, are all part of a comprehensive program’s success. Citizens can help reduce the spread of mosquito-borne diseases by following the 4Ds: Defend, Dress, Drain, and Dusk & Dawn. Applying an EPA-approved mosquito repellent and wearing close-toe shoes, light-colored clothing, and long sleeves and pants while outdoors can significantly protect you from mosquito bites. Draining any standing water that could be a potential mosquito breeding site significantly reduces the mosquito population and the application of insecticides. In addition, limiting your outdoor exposure time, especially from dusk to dawn when mosquitos are most active, will lessen your chances of being bitten. When a comprehensive IMM program is established, it will protect public health and keep our communities safe.

Importance of Integrated Mosquito Management
Our scientific experts at VDCI have the experience, knowledge, and equipment required to implement a comprehensive IMM plan. A proactive approach to mosquito surveillance reduces mosquito-borne diseases and provides adequate time to respond to disease threats before becoming a serious issue to the public. With our industry-leading experts guiding mosquito management strategies in the communities we serve, you can rest assured that your citizens are protected.
Contact Our Experts
Complete the form below to speak to an expert about your community’s mosquito management needs.
 Since 1992, Vector Disease Control International (VDCI) has taken pride in providing municipalities, mosquito abatement districts, industrial sites, planned communities, homeowners associations, and golf courses with the tools they need to run effective mosquito control programs. We are determined to protect the public health of the communities in which we operate. Our mosquito control professionals have over 100 years of combined experience in the field of public health, specifically vector disease control. We strive to provide the most effective and scientifically sound mosquito surveillance and control programs possible based on an Integrated Mosquito Management approach recommended by the American Mosquito Control Association (AMCA) and Centers for Disease Control and Prevention (CDC). VDCI is the only company in the country that can manage all aspects of an integrated mosquito management program, from surveillance to disease testing to aerial application in emergency situations.
Since 1992, Vector Disease Control International (VDCI) has taken pride in providing municipalities, mosquito abatement districts, industrial sites, planned communities, homeowners associations, and golf courses with the tools they need to run effective mosquito control programs. We are determined to protect the public health of the communities in which we operate. Our mosquito control professionals have over 100 years of combined experience in the field of public health, specifically vector disease control. We strive to provide the most effective and scientifically sound mosquito surveillance and control programs possible based on an Integrated Mosquito Management approach recommended by the American Mosquito Control Association (AMCA) and Centers for Disease Control and Prevention (CDC). VDCI is the only company in the country that can manage all aspects of an integrated mosquito management program, from surveillance to disease testing to aerial application in emergency situations.









 Without proper treatment, most dogs will die from heartworm disease which is why it’s important to monitor your dog and seek medical guidance if your dog is experiencing any of the symptoms associated with heartworms. Luckily, treatment is typically successful and prescription medicine can be used to prevent the development of heartworms should a dog be bitten by an infected mosquito. There are also FDA-approved products to prevent heartworms in dogs. Depending on the severity and stage of the disease, surgical removal may be necessary.
Without proper treatment, most dogs will die from heartworm disease which is why it’s important to monitor your dog and seek medical guidance if your dog is experiencing any of the symptoms associated with heartworms. Luckily, treatment is typically successful and prescription medicine can be used to prevent the development of heartworms should a dog be bitten by an infected mosquito. There are also FDA-approved products to prevent heartworms in dogs. Depending on the severity and stage of the disease, surgical removal may be necessary. In 80-90% of EEE cases, the infection is fatal, and horses may die within a few days. Luckily, vaccinations are available to protect horses from infection. While rare, EEE can also be contracted by humans. Treatment can be effective for less severe infections, but even with treatment, the disease is fatal in approximately 30% of cases.
In 80-90% of EEE cases, the infection is fatal, and horses may die within a few days. Luckily, vaccinations are available to protect horses from infection. While rare, EEE can also be contracted by humans. Treatment can be effective for less severe infections, but even with treatment, the disease is fatal in approximately 30% of cases.
 The claim likely originated from a study published in 1960 about how certain bats use echolocation to detect and capture small insects (Griffin et al. 1960). As part of the study, Donald Griffin and colleagues at Harvard University photographed little brown bats (Myotis lucifugus) and Eastern small-footed bats (M. leibii) preying on mosquitos (Culex quinquefasciatus) placed together in a room measuring (2.44 m. wide by 4.88 m. long by 2.44 m. tall (8 ft. wide by 16 ft. long by 8 ft. high). Only a small fraction of the bats (less than 10%) demonstrated prey capture behavior when released into the room that initially contained approximately 2000 mosquitoes, but the study focused on these “good catchers.” Again, this was a study on prey capture technique, not prey quantity.
The claim likely originated from a study published in 1960 about how certain bats use echolocation to detect and capture small insects (Griffin et al. 1960). As part of the study, Donald Griffin and colleagues at Harvard University photographed little brown bats (Myotis lucifugus) and Eastern small-footed bats (M. leibii) preying on mosquitos (Culex quinquefasciatus) placed together in a room measuring (2.44 m. wide by 4.88 m. long by 2.44 m. tall (8 ft. wide by 16 ft. long by 8 ft. high). Only a small fraction of the bats (less than 10%) demonstrated prey capture behavior when released into the room that initially contained approximately 2000 mosquitoes, but the study focused on these “good catchers.” Again, this was a study on prey capture technique, not prey quantity.

















 Since 1992, Vector Disease Control International (VDCI) has taken pride in providing municipalities, mosquito abatement districts, industrial sites, planned communities, homeowners associations, and golf courses with the tools they need to run effective mosquito control programs. We are determined to protect the public health of the communities in which we operate. Our mosquito control professionals have over 100 years of combined experience in the field of public health, specifically vector disease control. We strive to provide the most effective and scientifically sound mosquito surveillance and control programs possible based on an Integrated Mosquito Management approach recommended by the American Mosquito Control Association (AMCA) and Centers for Disease Control and Prevention (CDC). VDCI is the only company in the country that can manage all aspects of an integrated mosquito management program, from surveillance to disease testing to aerial application in emergency situations.
Since 1992, Vector Disease Control International (VDCI) has taken pride in providing municipalities, mosquito abatement districts, industrial sites, planned communities, homeowners associations, and golf courses with the tools they need to run effective mosquito control programs. We are determined to protect the public health of the communities in which we operate. Our mosquito control professionals have over 100 years of combined experience in the field of public health, specifically vector disease control. We strive to provide the most effective and scientifically sound mosquito surveillance and control programs possible based on an Integrated Mosquito Management approach recommended by the American Mosquito Control Association (AMCA) and Centers for Disease Control and Prevention (CDC). VDCI is the only company in the country that can manage all aspects of an integrated mosquito management program, from surveillance to disease testing to aerial application in emergency situations.